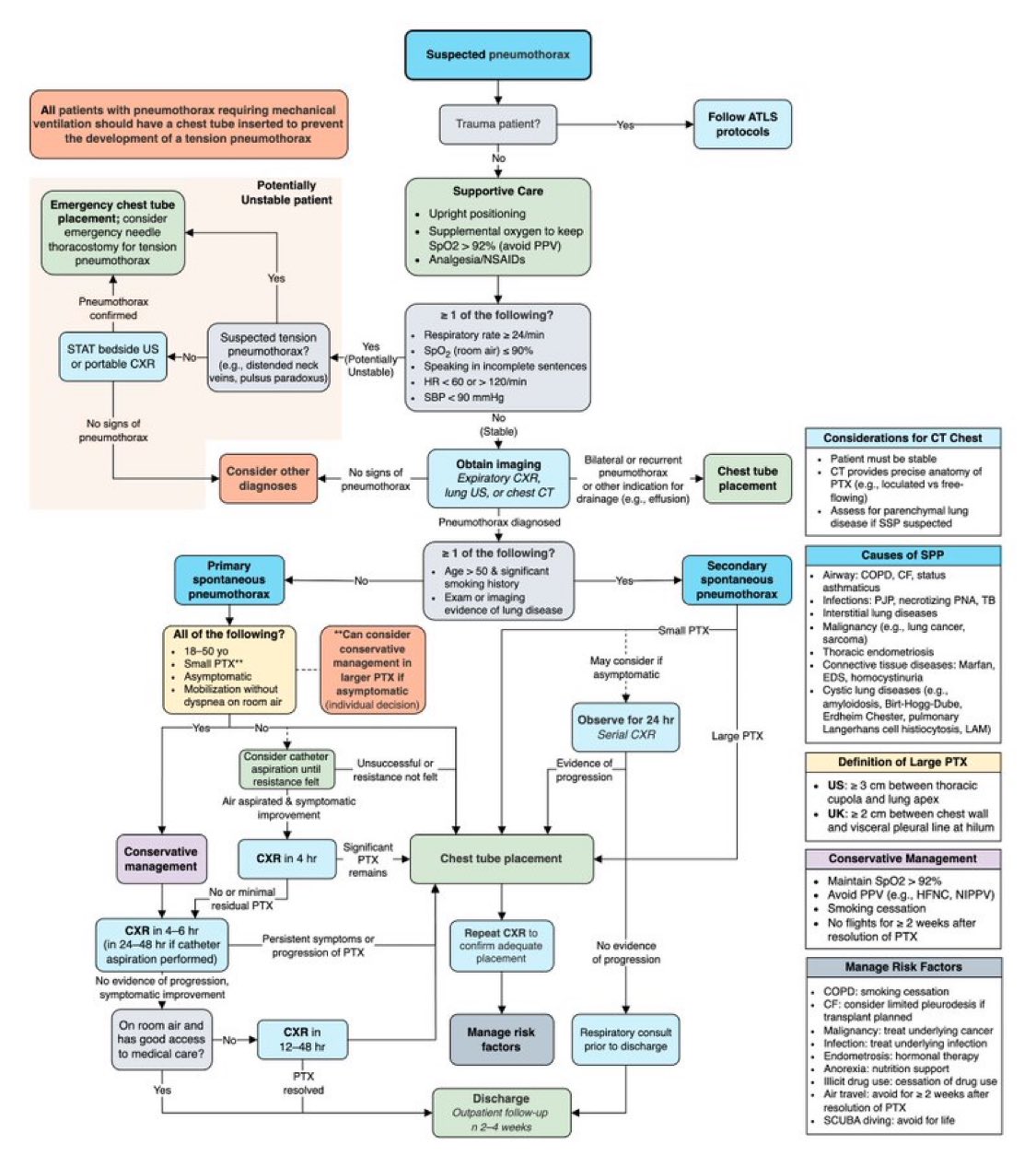
A pneumothorax (collapsed lung) occurs when air enters the pleural space, disrupting normal lung expansion. Early recognition and appropriate management are critical to prevent progression to tension pneumothorax, a life-threatening emergency. This post breaks down the systematic approach to pneumothorax evaluation and management.
Source
🔍 Step 1: Identify the Suspected Pneumothorax
Start with the clinical suspicion — typically triggered by symptoms such as sudden dyspnea, pleuritic chest pain, and decreased breath sounds.
If the patient has trauma, follow ATLS protocols.
For non-trauma cases, initiate supportive care:
- Upright positioning
- Supplemental oxygen (maintain SpO₂ > 92%; avoid PPV)
- Analgesia and NSAIDs
⚠️ Step 2: Assess Stability
A patient is potentially unstable if any of the following are present:
- Respiratory rate > 24/min
- SpO₂ < 90% on room air
- HR < 60 or > 120 bpm
- Systolic BP < 90 mmHg
- Difficulty speaking or signs of distress
If tension pneumothorax is suspected (e.g., distended neck veins, tracheal deviation, pulsus paradoxus):
👉 Perform emergency chest tube placement or needle decompression immediately.
Then confirm with bedside ultrasound or portable chest X-ray.
🫧 Step 3: Obtain Imaging for Stable Patients
For stable cases, obtain expiratory chest X-ray, lung ultrasound, or CT chest to confirm pneumothorax.
CT is reserved for:
- Recurrent or bilateral pneumothorax
- Suspicion of underlying lung disease (e.g., emphysema, bullae, fibrosis)
- Uncertain diagnosis
🧍 Step 4: Determine Type — Primary vs. Secondary
Primary Spontaneous Pneumothorax (PSP)
Occurs without underlying lung disease, often in tall, thin young males or smokers.
Criteria for conservative management:
- Age < 50 years
- Small pneumothorax
- Asymptomatic
- Able to ambulate without distress
If met, conservative care is reasonable:
- Observe with oxygen and repeat CXR in 4–6 hours
- If stable and improving → discharge with follow-up in 2–4 weeks
- If persistent or worsening → consider needle aspiration or chest tube
If aspiration fails or pneumothorax persists → Chest tube placement
Secondary Spontaneous Pneumothorax (SSP)
Occurs in patients with underlying lung disease (e.g., COPD, cystic fibrosis, TB, interstitial lung disease, lung cancer).
- Small SSP: Observe for 24 hours with serial CXR
- Large SSP or progression: Chest tube placement
- Manage comorbidities (e.g., stop smoking, address COPD)
- Respiratory consult before discharge
📏 Step 5: Define Pneumothorax Size
- US definition: > 3 cm between chest wall and lung margin at apex = large PTX
- UK definition: > 2 cm between chest wall and lung margin at hilum = large PTX
🩹 Step 6: Ongoing Management and Discharge
Conservative management includes:
- Maintaining SpO₂ > 92%
- Avoiding positive pressure ventilation
- Preventing recurrence (avoid air travel or SCUBA for 2–4 weeks after resolution)
Risk Factor Modification:
- Smoking cessation
- Avoid activities causing pressure changes
- Treat underlying lung diseases
💡 Takeaway
A systematic approach — assessing stability, underlying cause, and size — ensures timely, evidence-based management of pneumothorax.
Primary cases may resolve with observation, while secondary or unstable cases require immediate intervention.