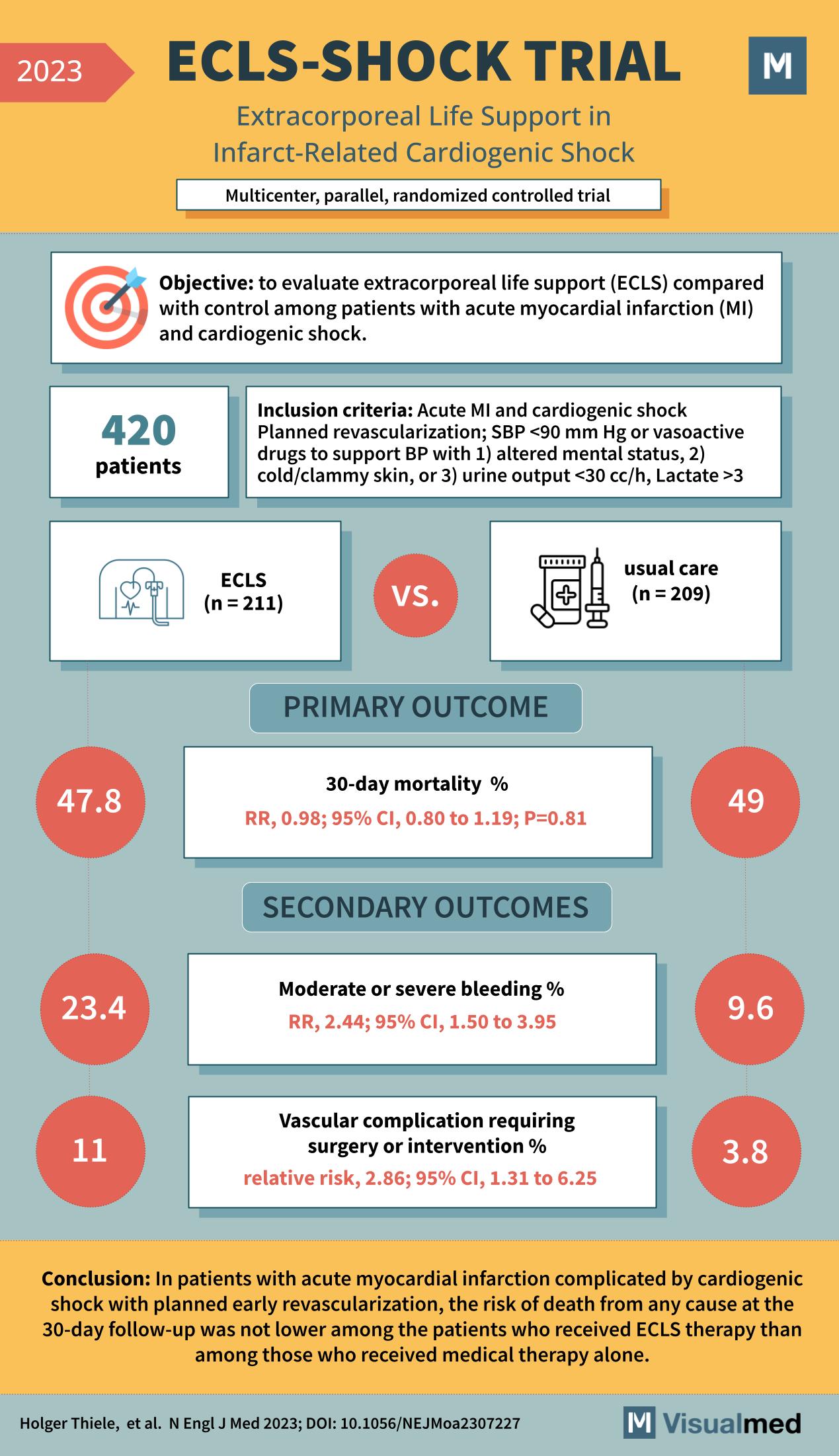
The ECLS-SHOCK trial, as reported in the New England Journal of Medicine in 2023, was a multicenter, parallel, randomized controlled trial designed to evaluate the efficacy of extracorporeal life support (ECLS) in patients with acute myocardial infarction (MI) complicated by cardiogenic shock.
The study included 420 patients who met the criteria of acute MI and cardiogenic shock, had planned revascularization, and required support for blood pressure (BP) due to symptoms such as altered mental status, cold/clammy skin, or reduced urine output. Patients were randomized into two groups: those receiving ECLS (n=211) and those receiving usual care (n=209).
The primary outcome was 30-day mortality, with the ECLS group showing a 47.8% mortality rate compared to a 49% rate in the usual care group. The relative risk (RR) was 0.98, indicating no significant difference between the groups (95% CI, 0.80 to 1.19; P=0.81).
Secondary outcomes included the incidence of moderate or severe bleeding and vascular complications requiring surgery or intervention. The ECLS group had a higher incidence of bleeding (23.4%) than the usual care group (9.6%), with a significant RR of 2.44 (95% CI, 1.50 to 3.95). Vascular complications were also more common in the ECLS group (11%) compared to the usual care group (3.8%), with a relative risk of 2.86 (95% CI, 1.31 to 6.25).
The conclusion drawn from the ECLS-SHOCK trial was that in patients with acute myocardial infarction complicated by cardiogenic shock and planned early revascularization, the risk of death at 30 days was not lower among those who received ECLS therapy compared to those who received medical therapy alone.
The implications of the ECLS-SHOCK trial are significant for clinical practice in the management of patients with cardiogenic shock. While ECLS did not demonstrate a survival benefit, it is important to note the increased risk of bleeding and vascular complications associated with the therapy. The study highlights the need for careful patient selection and management strategies when considering ECLS for those with severe cardiovascular complications.