DEVICE Trial Summary
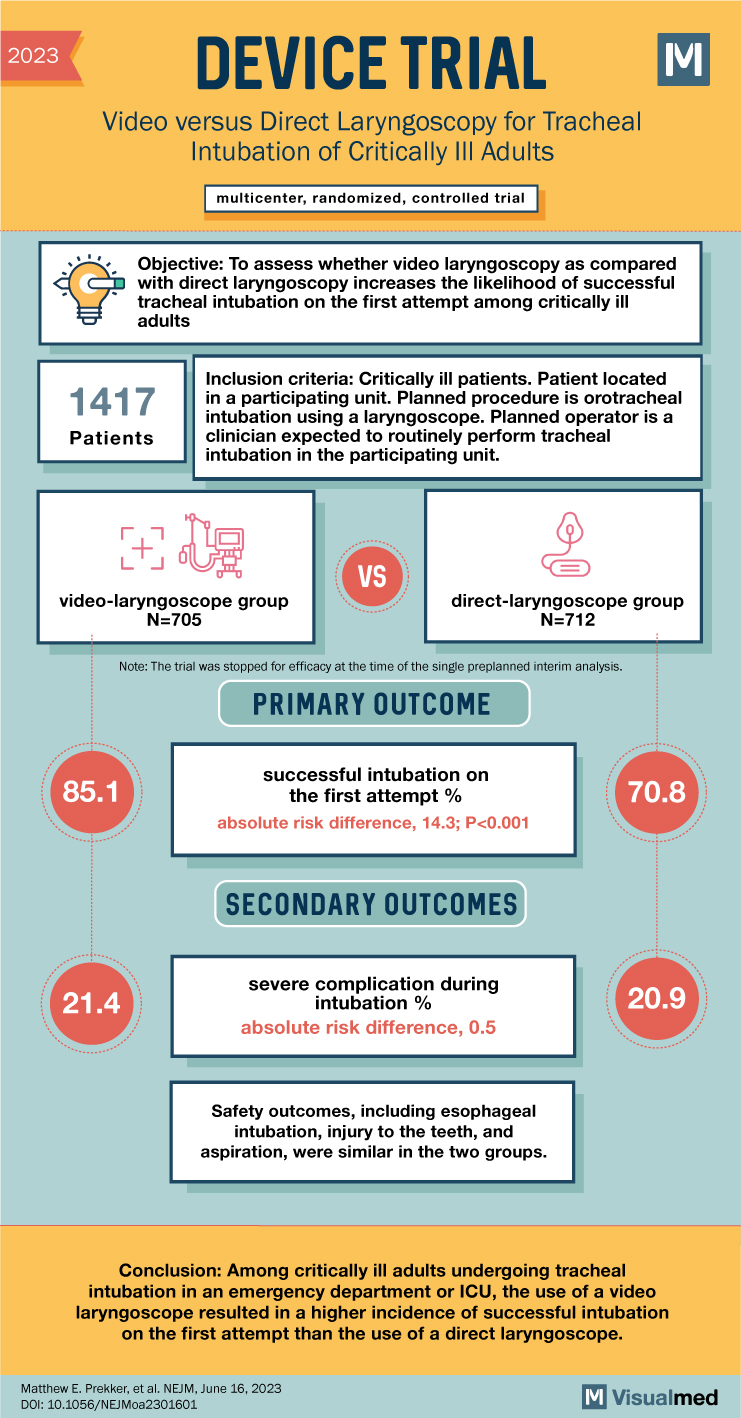
The article discusses the findings of the DEVICE trial, which aimed to determine whether video laryngoscopy increased the likelihood of successful tracheal intubation on the first attempt compared to direct laryngoscopy in critically ill adults.
The trial was conducted at 17 emergency departments and intensive care units (ICUs), involving a multicenter, randomized design. Critically ill adults undergoing tracheal intubation were randomly assigned to either the video-laryngoscope group or the direct-laryngoscope group. The primary outcome assessed was successful intubation on the first attempt, while the occurrence of severe complications during intubation was considered a secondary outcome. Severe complications were defined as severe hypoxemia, severe hypotension, new or increased use of vasopressors, cardiac arrest, or death.
The trial was stopped for efficacy at the preplanned interim analysis. The final analysis included 1,417 patients, with 91.5% of them undergoing intubation performed by an emergency medicine resident or a critical care fellow. The results indicated that successful intubation on the first attempt occurred in 85.1% of patients in the video-laryngoscope group and 70.8% of patients in the direct-laryngoscope group. This represented an absolute risk difference of 14.3 percentage points, with a statistically significant difference between the groups (P<0.001).
Regarding severe complications during intubation, 21.4% of patients in the video-laryngoscope group and 20.9% in the direct-laryngoscope group experienced such complications. The absolute risk difference was 0.5 percentage points, with the 95% confidence interval indicating no significant difference between the two groups (−3.9 to 4.9). Safety outcomes, including esophageal intubation, injury to the teeth, and aspiration, were similar in both groups.
In conclusion, the DEVICE trial demonstrated that among critically ill adults undergoing tracheal intubation in emergency departments or ICUs, the use of a video laryngoscope resulted in a higher incidence of successful intubation on the first attempt compared to the use of a direct laryngoscope. This finding suggests that video laryngoscopy may be a beneficial tool in improving first-attempt intubation success rates in critically ill patients. The study did not show a significant difference in severe complications between the two groups. Safety outcomes were comparable, suggesting that the use of a video laryngoscope does not pose an increased risk of adverse events compared to a direct laryngoscope. These results provide valuable insights for clinicians and highlight the potential advantages of incorporating video laryngoscopy into tracheal intubation procedures for critically ill adults.