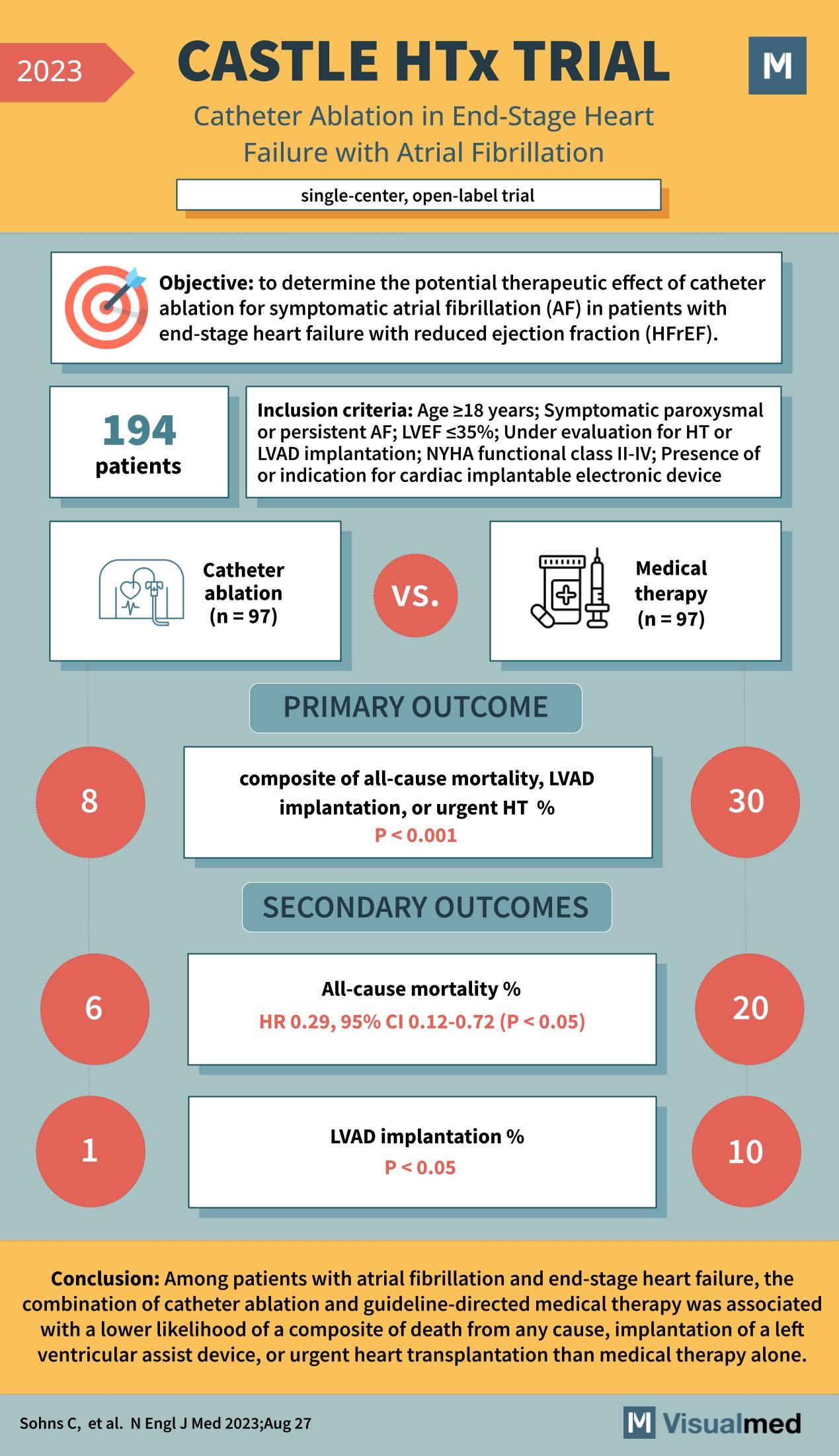
The CASTLE HTx trial, as published in the New England Journal of Medicine in 2023, was a single-center, open-label trial that aimed to determine the potential therapeutic effect of catheter ablation for symptomatic atrial fibrillation (AF) in patients with end-stage heart failure with reduced ejection fraction (HFrEF).
This trial enrolled 194 patients who met the inclusion criteria, such as being 18 years or older, having symptomatic paroxysmal or persistent AF, an ejection fraction of less than 35%, and being under evaluation for heart transplantation (HT) or left ventricular assist device (LVAD) implantation. Patients were randomized to receive either catheter ablation (n=97) or medical therapy (n=97).
The primary outcome was a composite of all-cause mortality, LVAD implantation, or urgent heart transplantation. The results showed that 8% of the catheter ablation group reached this composite endpoint compared to 30% of the medical therapy group, with a p-value of less than 0.001, indicating a significant benefit of catheter ablation.
Secondary outcomes included all-cause mortality and LVAD implantation percentages. All-cause mortality in the catheter ablation group was 6% compared to 20% in the medical therapy group, with a hazard ratio (HR) of 0.29, suggesting a significant mortality reduction with ablation (95% CI, 0.12-0.72; P < 0.05). LVAD implantation was also lower in the ablation group (1%) compared to the medical therapy group (10%), with a p-value of less than 0.05.
The conclusion of the CASTLE HTx trial was that among patients with atrial fibrillation and end-stage heart failure, the combination of catheter ablation and guideline-directed medical therapy was associated with a lower likelihood of a composite of death from any cause, implantation of a left ventricular assist device, or urgent heart transplantation than medical therapy alone.
This trial provides significant evidence supporting the use of catheter ablation as a beneficial intervention for patients with AF and advanced heart failure, potentially impacting future guidelines and treatment strategies in this high-risk patient population.